The mouth-body connection – raising awareness of how gum disease and systemic diseases are linked.
Author: Eimear Staunton, Dental Hygienist, Dublin
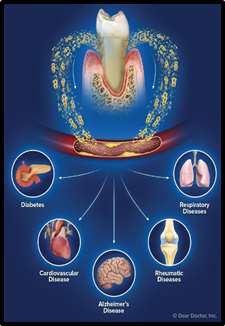
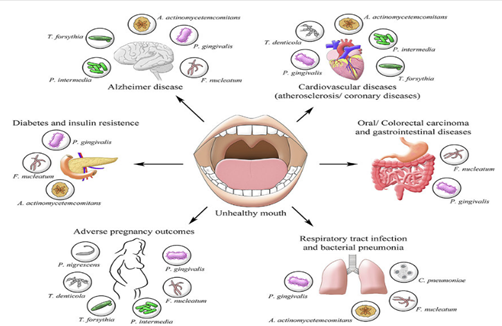
As dental hygienists, our role in healthcare is vital in the prevention of both oral and systemic diseases. Our job can sometimes be underestimated as just a routine cleaning procedure but our patients are not always aware that periodontal disease, commonly known as gum disease, is linked to many life-altering systemic diseases like diabetes, cardiovascular disease, cancer and Alzheimer’s disease. It can also be linked to respiratory and rheumatic disease, premature birth rates and infertility. Everyday we are working in the treatment and prevention of gum disease, screening for signs of oral cancer, and making a valuable difference not only to the oral health of our patients but also to their overall systemic health and wellbeing.
We have all heard the old adage that the mouth is the gateway to the body and right now during this Covid-19 pandemic, these words have never been more relevant. In February 2021, a clinical study published by the Journal of Clinical Periodontology found a connection between gum disease and the severity of Covid-19 infections. The results of this study found that more than 80% of Covid-19 patients with severe complications had gum disease. These patients had higher inflammatory markers than those without. They found that patients with gum disease were 4.5 times more likely to need a ventilator, 3.5 times more likely to be sent to ICU and 9 times more likely to die from Covid-19. This study demonstrates that there is a pathophysiology that links the mouth to systemic diseases involving chronic inflammation and an altered immune response.
Periodontal disease is a destructive inflammatory disease of the gums and surrounding bone. It is the biggest cause of tooth loss in the adult population and according to a study by the Centers for Disease Control and Prevention, nearly half of American adults age 30 and older and 70% of those 65 and older have some degree of gum disease. As gum disease is often painless and symptoms are subtle, patients are often unaware of the irreversible degeneration taking place. Gum disease is largely preventable and risk factors for developing it include poor oral hygiene, genetics, smoking, stress, age, type II diabetes and some medications.
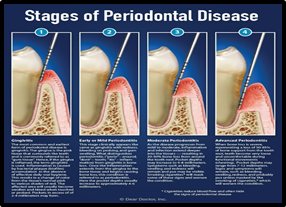
It is important to note that the risk factors for gum disease are also the same shared risk factors for many systemic diseases and more research is needed to fully understand and establish what the cause-and-effect relationship is between them. One connection we know is via harmful bacteria in the mouth which enters the bloodstream through the gums after brushing, flossing, trauma or surgical procedures and can travel to other parts of the body where it can release toxins and cause disease to occur. A growing body of research suggests that the most common thread between many systemic conditions and gum disease is inflammation. Gum disease is the most common chronic inflammatory disease in humans. Inflammation is essential for healing however when it becomes chronic and persists over a long time even at a low level it becomes damaging to the body. Ongoing research is fundamental to understanding how the detrimental effects of oral inflammation on the body can increase the risk of developing systemic diseases.
Diabetes
Epidemiological research over many decades has shown diabetes is a major risk factor for developing gum disease. Diabetes has a bidirectional relationship with gum disease in that a diabetic patient is more likely to have gum disease and visa-versa. There is also strong evidence that treating one improves the other. The risk of gum disease in people with diabetes is 200-300% more than those without diabetes. Correspondingly, gum disease may make it more difficult for people who have diabetes to effectively control their blood sugar levels. Effective treatment of gum disease in patients with type II diabetes has shown to reduce blood glucose levels (HbA1c) by 0.3-0.4% after 3-4 months, the equivalent of adding a second line drug in the management of their diabetes. In addition, improving oral health has also shown to reduce diabetic associated complications including cardiovascular disease, kidney disease, visual impairment, limb loss and peripheral nerve damage.
Cardiovascular disease
Many recent studies indicate that gum disease and cardiovascular disease are associated and that having gum disease increases the risk of developing cardiovascular disease. Both are chronic inflammatory conditions and it is thought the main connection is from the migration of harmful bacteria. The oral bacteria associated with gum disease were found in arterial plaque deposits that accumulate on the walls of blood vessels. When these bacteria reach the heart, they can attach themselves to damaged areas and cause inflammation. This can result in illnesses such as endocarditis, an infection of the inner lining of the heart. According to the American Heart Association, other cardiovascular conditions such as atherosclerosis (clogged arteries) and stroke have also been linked to inflammation caused by oral bacteria.
Cancer
Research published in The Lancet Oncology which studied 48,375 men over 17 years, concluded that men with a history of gum disease are 14% more likely to develop cancer than men with healthy gums. More specifically, researchers found that men with gum disease were 49% more likely to develop kidney cancer, 54% more likely to develop pancreatic cancer, and 30% more likely to develop blood cancers. The cancer risk persisted in those who never smoked tobacco. A 2016 study published by the Journal of Periodontology which looked at 5 cohort studies involving 321,420 participants investigated the link between gum disease and lung cancer. There is a correlation in that we already know that smoking is a risk factor for developing both gum disease and lung cancer. Researchers separated participants with a history of tobacco and alcohol use from participants who never used tobacco and had low alcohol consumption. They found that there was still an increased risk in non-tobacco using participants meaning that even with no other risk factors involved, having gum disease alone increased their risk of developing lung cancer. In addition to lung cancer, studies have pointed to gum disease having links with colorectal and gastrointestinal cancer. Fusobacterium nucleatum, a bacteria specific to gum disease was found in malignant tissue samples from colorectal cancer patients. In a healthy mouth F. nucelatum is not problematic but in cases of poor oral hygiene, uncontrolled diabetes and other systemic conditions, it can go rogue and cause gum disease, tonsillitis, appendicitis and even premature births. Many studies over the last decade found F.nucleatum DNA present in tumor cells. In this instance, patients with pancreatic, colorectal and esophageal cancer had a poorer prognosis and there was a resistance to chemotherapy in colorectal and esophageal cancer patients. This bacterium can trigger changes in some primary colorectal tumors that lead to dangerous metastasis (spread of cancer to new areas of the body). According to the WHO, colorectal cancer is the world’s third most common cancer and second deadliest malignancy.
Alzheimer’s disease
A 2019 study, published in the Journal of Sciences Advanced, discovered a potential link between Porphyromonas gingivalis, a bacteria associated with gum disease and Alzheimer’s disease. This study analysed brain tissue, spinal fluid, and saliva from Alzheimer’s patients and found the presence of P. gingivalis in these samples. Gingipains, a toxic enzyme secreted by P. gingivalis was detected in 96% of the brain tissue samples examined. Furthermore, researchers noted that the presence of P. gingivalis increased the production of amyloid plaques whose accumulation contributes to Alzheimer’s disease. Via animal testing, the study confirmed that P. gingivalis can travel from the mouth to the brain and that the gingipains it secretes can destroy brain neurons. These findings are very significant as they suggest a biological mechanism for bacteria specific to gum disease to contribute to the development and progression of Alzheimer’s disease. An observational study also found a notable decline in cognition over a 6-month period compared to Alzheimer’s patients without active gum disease. A 2017 study of 25,000 participants published in Alzheimer’s Research & Therapy found that people who suffered from gum disease for ten years or more, were up to 70% more likely to develop Alzheimer’s disease.
Respiratory disease
Research suggests that gum disease is a risk factor for developing respiratory diseases including chronic obstructive pulmonary disorder (COPD), chronic bronchitis, emphysema and pneumonia. The anatomical continuity between the oral cavity and the lungs means that there is a two-way relationship when it comes to bacterial migration. Harmful bacteria associated with gum disease can be inhaled into the lungs, causing respiratory infections and correspondingly respiratory pathogens can migrate and colonise in the oral cavity and can be difficult to eradicate. Although smoking is the biggest risk factor for developing respiratory diseases, gum disease plays a significant role. According to the American Thoracic Society, gum disease can also worsen the chronic inflammation in lung diseases such as asthma and COPD. Inflammation in the airways leads to more frequent symptoms and lung damage.
Rheumatic disease
Rheumatic diseases are autoimmune and inflammatory diseases that cause the immune system to attack joints, muscles, bones and organs. One of the most commonly known rheumatic diseases is the chronic, joint-destroying autoimmune disease rheumatoid arthritis (RA). Since the early 1900’s, researchers believed there could be a clinical association between gum disease and arthritis. A study in 2012 9 found that RA patients were four times more likely to have gum disease than those without RA and their gum disease was often more severe. A 2017 study from the Johns Hopkins University Division of Rheumatology 10 found evidence that a bacterium associated with chronic gum disease, Aggregatibacter actinomycetemcomitans (Aa) was found in the joints of patients with RA. Researchers suspected that both diseases may be triggered by a common factor. This study identified a process occuring in the gums of patients with active gum disease which has also been observed occuring in the joints of patients with RA called hypercitrullination. Citrullination is a process that occurs naturally in everyone to regulate the function of proteins. In people with RA, this process becomes overactive which results in hypercitrullination and the abnormal accumulation of citrullinated proteins. This increases the production of antibodies against these proteins which creates inflammation and attacks the joints in patients with RA. The study identified that the periodontal bacteria (Aa) which was found in the joints of people with RA, could trigger hypercitrullination in white blood cells confirming a longstanding link between these two conditions. Understanding how this process causes the immune system to attack may lead to breakthroughs into how to treat RA in the future. Furthermore, a study by researchers at Case Western University published in the
Journal of Periodontology in 2009 11 found that when people with a severe form of rheumatoid arthritis successfully treated their gum disease, their pain and other arthritis symptoms improved.
It is important for all dental professionals to keep updated with ongoing research of how these systemic diseases are linked to oral health in order to inform and correctly advise our patients and improve their quality of life for the long term. It will also be important for medical teams to liaise with dental teams in order to dually treat and manage the conditions.
What to do…
- See your dentist for a general check-up annually.
- Attend your dental hygienist every 6 months for a scale and polish, if you have gum disease you will be recommended to attend 3-4 monthly.
- Make good oral hygiene a daily habit by brushing twice a day for two minutes with a fluoride toothpaste and interdental cleaning with dental floss or interdental brushes at least once per day.
- Know the common signs of gum disease, these include swollen gums, bleeding on brushing or flossing, bad breath, a build-up of tartar, receding gums, loose teeth or teeth starting to drift.
- Stop smoking as this is a major risk factor for gum disease.
- Maintain a healthy balanced diet. A recent study suggested an “anti-inflammatory diet” low in refined carbohydrates and rich in whole grains, Omega-3 fatty acids, vitamins C and D, antioxidants, and fiber can help control gum disease. Reduce snacking on sugary foods and drinks.
- Keep active to maintain a healthy weight to prevent diabetes and other systemic diseases.
References
Available upon request.